
Chronic prostatitis is a serious problem. Even modern urology is not able to answer many questions about this pathology. Experts believe that chronic prostatitis is a disease that is the result of a whole range of health problems, including tissue damage, as well as dysfunctions not only of the urinary and prostate glands, but also of other organs.
The pathology is mainly diagnosed in men of reproductive age. In older men, chronic prostatitis is often accompanied by benign prostate tumors.
Classification of diseases
The classification of prostatitis was developed by scientists at the US National Institutes of Health in 1995:
%20and%20inflammatory%20chronic%20prostatitis%20(right).webp)
- 1 type- acute bacterial prostatitis. It is diagnosed in 5% of cases of prostate inflammation.
- type 2- bacterial chronic prostatitis.
- 3 type- chronic bacterial prostatitis. This pathology has another name - chronic pelvic pain syndrome.
- type 3A- an inflammatory form of chronic prostatitis. It is diagnosed in 60% of cases of chronic prostatitis.
- type 3B- non-inflammatory form of chronic prostatitis. It is diagnosed in 30% of cases.
- 4 type- asymptomatic prostatitis.
There is also a classification of chronic prostatitis, compiled in 1990.
Symptoms of chronic prostatitis
Discomfort and pain in the pelvic area lasting more than 3 months are the main symptoms of chronic prostatitis.
In addition, urinary disorders and erectile dysfunction are observed:
- pain occurs in the perineum, may radiate to the anus, groin, inner thigh, sacrum, waist and scrotum. Pain on one side, extending to the testicle, is often not a symptom of chronic prostatitis.
- no erection occurs despite the presence of suitable conditions, but complete impotence is not observed.
- in the early stages of the disease, premature ejaculation is observed.
- Frequent urination, urinary incontinence, pain and burning during the process of emptying the bladder.
The clinical picture may differ depending on the type of chronic prostatitis.
infectious form:
- Frequent urination at night.
- Pain in the thighs, perineum, glans penis and rectum, aggravated by movement.
- painful urination;
- poor urine flow.
Particularly infectious:
- mucous discharge from the urethra.
- the above symptoms.
Non-infectious prostatitis:
- acute pain in the perineum.
- pain in the thighs and head of the penis.
- the pain is intensified by the forced cessation of sexual intercourse or the prolonged absence of a close life.
Great!The disease progresses in waves. The symptoms can either weaken or intensify, but their presence clearly indicates the presence of an inflammatory process.
Symptoms may vary depending on the stage of the pathology.

The following stages of development of the pathology can be distinguished:
- Exudative.The patient feels pain in the pubic, groin and scrotum. There is frequent urination and discomfort after intercourse. An erection can hurt.
- Alternative solution.The pain intensifies, is located in the groin, the pubic area and gives to the sacrum. Urination accelerates, but occurs without difficulty. Erection does not suffer.
- Multiplication.During an exacerbation, urination becomes more frequent. Urine flow becomes weak.
- Cicatricial.Prostate tissue hardening occurs. There is a feeling of heaviness in the sanctuary and pubic area. Increased urination. The erection becomes weak. Ejaculation may be completely absent.
The symptoms may vary depending on the course of the disease, but in each case, they will increase gradually.
Causes of chronic prostatitis
There are many factors that lead to chronic prostatitis. The disease occurs under the influence of infectious agents. The patient has hormonal, neuroblastic, immune and hemodynamic disorders. Biochemical factors, the reflux of urine into the prostate lobes and the dysfunction of growth factors, which are responsible for the proliferation of living cells, affect.
Reasons that affect the formation of pathology:
- urogenital infections.
- weakness;
- irregular sex life;
- continuous catheterization of the bladder.
- regular hypothermia.
Developmentdiseases of a bacterial naturepromotes intraprostatic reflux of urine.
Chronic bacterial prostatitisdevelops in the context of neurogenic disorders of the pelvic floor muscles, as well as elements that are responsible for the function of the bladder wall, prostate and urethra.
Formationmyoperitoneal activation points, located near the organs of the urogenital system and the prostate gland, can cause pelvic pain syndrome. Signs that are the result of certain diseases, surgeries and injuries can cause pain in the genital area, perineum and adjacent areas.
Diagnosis of pathology
The presence of a complex of symptoms makes it possible to diagnose chronic prostatitis without much difficulty. However, in some cases, the pathology may be asymptomatic. In this case, in addition to the formal examination and interrogation of the patient, additional research methods are required.Neurological examination and study of the patient's immune status is mandatory..
Great!Special questionnaires and questionnaires allow you to more accurately identify the patient's subjective feelings and get a complete picture of the state of health, the intensity of pain, ejaculatory disorders, erection and urination.
Laboratory diagnosis
Laboratory diagnosis makes it possible to distinguish between a bacterial and bacterial form of pathology, as well as to determine the type of pathogen and the most accurate diagnosis.Chronic inflammation of the prostate is confirmed when the fourth urine sample or prostate secretion contains more than 10 leukocytes in the PZ or bacterial compounds.When the white blood cell count is high but the bacteria have not spread, the material is tested for chlamydia or other STD pathogens.
- The urethral secretion is sent to the laboratory to detect viral, fungal and bacterial flora, leukocytes and mucus in it.
- Scratching from the urethra is examined by PCR. This allows you to identify sexually transmitted pathogens.
- Perform a microscopic examination of prostate secretion to count the number of macrophages, leukocytes, amyloid and Trousseau-Lalemand bodies. An immunological study and a bacteriological study are prescribed. Determine the level of non-specific antibodies.
- The blood sample is taken ten days after the digital rectal examination to determine the concentration of PSA in it. At a rate above 4. 0 ng / ml, the patient undergoes a prostate biopsy to rule out oncological examination.
The diagnosis is made based on the results of the research.
Instrumental diagnosis

Corrective gland ultrasound will help to clarify the stage and form of the disease. Ultrasound allows you to rule out other diagnoses, monitor the effectiveness of treatment, as well as determine the size of the prostate, its sound structure, the homogeneity and density of the seminal vesicles. Urodynamic studies and myography of the pelvic floor muscles will allow the detection of subclavian obstruction and neurogenic disorders that often accompany the pathology.
Tomography and magnetic resonance imaging are used for the differential diagnosis, especially with prostate cancer. These methods will reveal violations in the pelvic organs and spine.
Differential diagnosis
Differential diagnosis is important, as there is a risk that the patient will have a more serious illness.
Differential diagnosis is made with such diseases:
- pseudodynamic dysfunction, functional disorder of the extruder-sphincter system, bladder dysfunction of neurogenic origin, complex peripheral pain syndrome.
- stenosis of the bladder, hypertrophic changes in the bladder neck, prostate adenoma.
- pubic osteoarthritis, cystitis.
- pathology of the rectum.
If symptoms occur, the prostate gland should be examined by a urologist or andrologist. Have an ultrasound. If necessary, a prostate gland biopsy is prescribed.
Pathology treatment methods
Chronic prostatitis is treated by a urologist or andrologist. The treatment is performed in a complex way. The correction depends on the patient's lifestyle, thinking characteristics and habits. It is important to exercise more, minimize alcohol intake, get rid of nicotine addiction, eat right and normalize your sex life. However, doing without a course of basic treatment will not work. Taking medication is the main condition for complete recovery.
Indications for hospitalization
Most often, the treatment is performed on an external basis. However, in cases where the disease can not be corrected and has a tendency to recur, the patient is referred to a hospital where treatment is most effective.
Medical method of treatment
This method aims to eliminate the existing infection, to normalize blood circulation, to improve the drainage of the prostate lobes, to correct the hormonal background and the immune status. Therefore, doctors prescribe antibiotics, vasodilators, immunomodulators, anticholinergics and anti-inflammatory drugs.
If the pathology is bacterial in nature, antibiotics are definitely recommended. The agent is prescribed based on the results of bacterial prostate secretion culture.This will make it possible to isolate the pathogen by subsequently determining its susceptibility to a particular drug. With a well-designed regimen, the effectiveness of the treatment reaches over 90%.
In the bacterial form, a short course of antibiotics is prescribed. Continue only if the pattern gives a positive result. The effectiveness of the treatment is about 40%
With chronic pelvic pain, the course of antibiotics is no longer than one month. With positive dynamics the treatment continues for another month. If there is no effect, the drug is replaced by another, which may be more effective.
Antibacterial agents from the fluoroquinolone group are the main drugs for the treatment of pathology.They have high bioavailability, are active against most gram-negative bacteria, ureaplasmas and chlamydia, accumulate in prostate tissues.
When treatment with fluoroquinolones is not effective, penicillins may be prescribed.
Antibacterial drugs are used for preventive purposes.
Following treatment with antibiotics, treatment with α-blockers is prescribed.This treatment strategy is effective for patients who have persistent obstructive and irritating symptoms.
If urinary incontinence and pain persist, tricyclic antidepressants may be prescribed, which have analgesic effects.
With severe urinary incontinence, a urodynamic study is performed prior to treatment and is performed based on the results obtained.
Non-drug treatment
Drug-free treatments make it possible to increase the concentration of antibacterial drugs in the glandular tissues, but overdose is not recommended.
The following methods are used for this purpose:
- electrophoresis?
- Laser treatment?
- Voiceover?
- Microwave hyperthermia (applied correctly).
When applying the latter method, the temperature is selected separately. The temperature, set in the range of 39-40 degrees, allows you to increase the concentration of the drug in the body, activates the immune system at the cellular level, eliminates bacteria, relieves congestion. Increasing the range to 40-45 degrees allows you to achieve a hardening and analgesic effect.
Laser and magnetic therapy are used in combination. The result is similar to the result of the above methods, but also has a biostimulatory effect on the organ.
Corrective massage is performed only in the absence of contraindications.
Surgical method
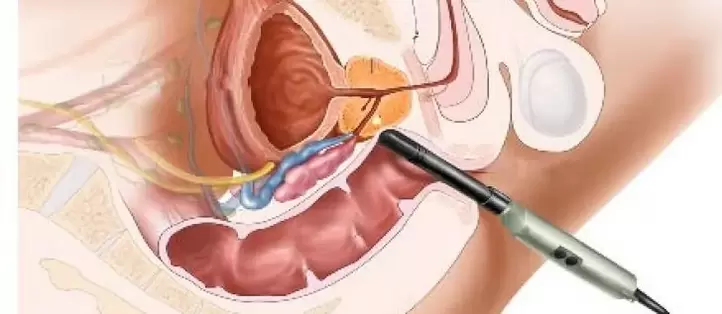
Chronic prostatitis generally does not require surgery. Exceptions are complications that pose a threat to the patient's health and life. Modern surgical treatment allows the use of endoscopic surgery. It is minimally invasive. Recovery is faster and causes minimal damage to the body.
The surgical method is prescribed for:
- prostate sclerosis;
- prostate adenoma;
- hardening of the seed tubercle.
- prostate calcification.
Great!Surgery is contraindicated in the acute stage. Surgical treatment is prescribed by the surgeon based on the results of the study and the overall clinical picture.
Prognosis for chronic prostatitis
Doctors are skeptical about predicting the outcome of the disease. It is rare to achieve complete recovery. Basically, chronic prostatitis goes into a stage of long-term remission. The symptoms disappear, the number of urine and blood returns to normal. In order not to make chronic prostatitis more active and to cause complications, it is necessary to follow all the recommendations of a specialist.

























